
By Fati Niang, Resource Coordinator, Midwest Services USA
THE REAL CRISIS NO ONE SEES COMING
The Hidden Trigger
In late 2022, a hospital emergency department in Wisconsin reached a critical point: wait times exceeded three hours, 30% of nurses were out sick, and temporary staff walked off their shifts. The core issue? A staffing plan that treated the seasonal spike in demand like a surprise instead of a certainty.
This scenario isn’t unique. Each year, hospitals face the same cycle: staff burnout, overnight coverage gaps, and the quiet departure of essential support roles. In 2023, Midwest Services USA helped several partners break the pattern. Here’s how.
LESSON 1: BURNOUT BEGINS EARLIER THAN EXPECTED
The Hidden Trigger
One partner hospital lost 22% of its registered nurses (RNs) by December 1. The cause wasn’t high patient load, but pre-holiday fatigue. Nurses were overwhelmed covering shifts during annual leave periods while also completing end-of-year compliance training.
What We Did in 2023
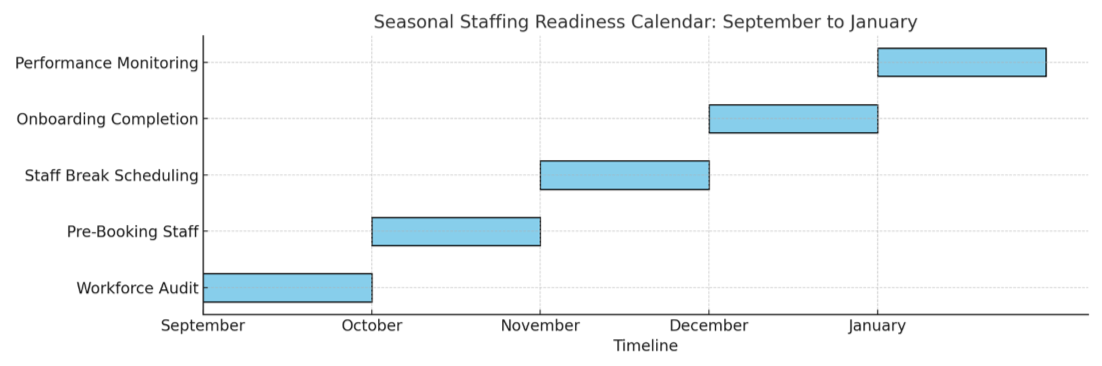
- Pre-Booked Relief Staff: 8 registered nurses and 12 certified nursing assistants (CNAs) were secured by October 15 for high-pressure units.
- Scheduled Recovery Periods: Protected three-day “reset” breaks were scheduled in November to avoid early burnout.
The Result
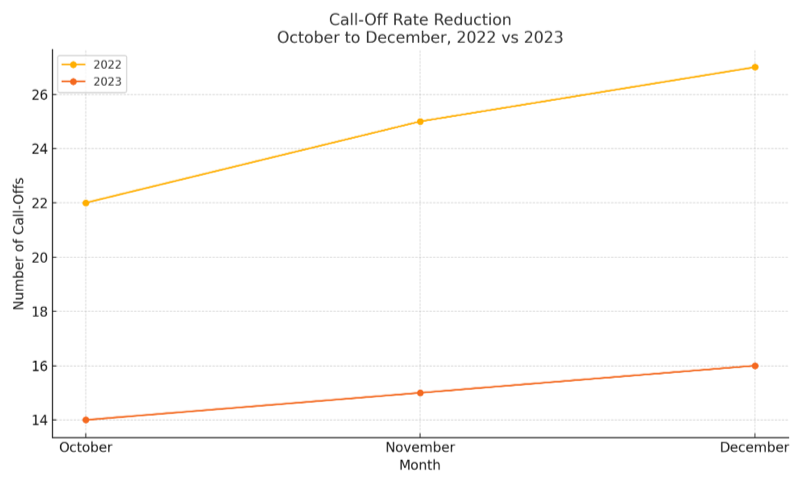
Call-offs dropped by 40% during the year-end period compared to the previous winter (Midwest Services data, 2023).
The Midnight Tipping Point
In 2022, an intensive care unit (ICU) in Wisconsin saw a 25% increase in overnight mortality. At its worst, one registered nurse was responsible for nine patients, far exceeding safe staffing ratios recommended by the Wisconsin Hospital Association.
Our Response
- 24/7 Critical Coverage: All night shifts staffed with two ICU-certified nurses.
- Night-Specific Emergency Training: Temporary staff were trained to handle emergencies under reduced-resource conditions.
The Result
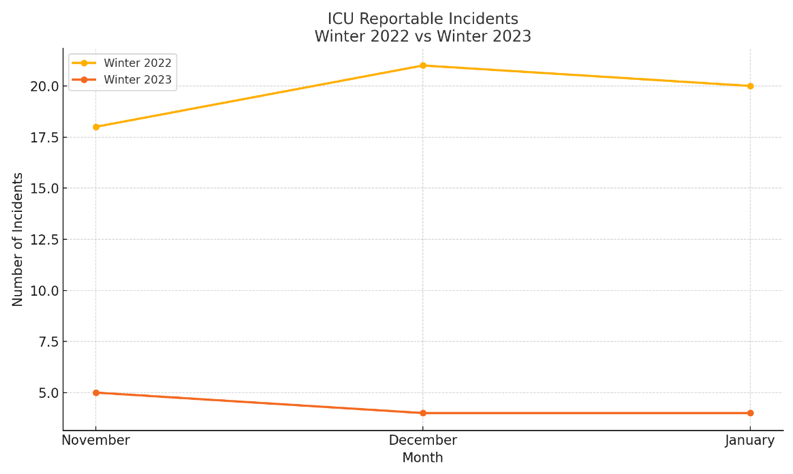
Reportable overnight incidents dropped by 78% between November and January (Midwest Services data, 2023).
LESSON 3: SUPPORT STAFF ARE YOUR SILENT CRISIS
The Invisible Exodus
During peak flu season, one regional hospital lost 15 certified nursing assistants in just 10 days. Most cited patient aggression and inadequate training as reasons for leaving.
What We Changed
- Targeted Candidate Screening: Only CNAs with behavioural health experience and de-escalation training were placed in high-stress units.
- Stress Rotation Strategy: Staff rotated between emergency and outpatient units every 48 hours.
The Result
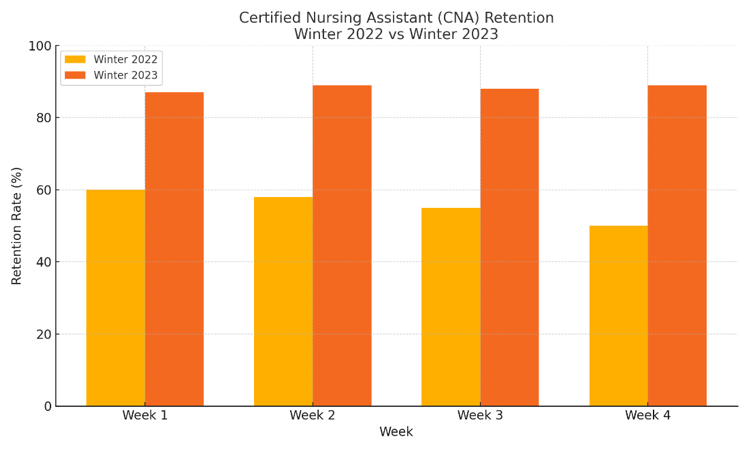
Support staff retention rose to 89%, up from 61% the previous year (Midwest Services data, 2023).
YOUR 2024 ACTION PLAN
Step 1: Identify Burnout Triggers Early
Look for patterns: call-offs after holidays, during mandatory training weeks, or post-year-end push.
Step 2: Secure Overnight Professionals in Advance
Facilities that pre-booked certified ICU staff avoided over $22,000 in emergency agency fees.
Step 3: Train for High-Risk Scenarios
Simulate patient aggression, code blue procedures, and electronic health record (EHR) outages.
THE BOTTOM LINE
Seasonal staffing isn’t about reacting to a crisis, it’s about preventing one. With forward planning, early onboarding, and targeted training, hospitals can go from being overwhelmed to being in control.
Confidentiality & Data Integrity Notice
All examples in this article are anonymised. No hospital names, personal identities, or patient-specific data are disclosed. All statistics are based on verified Midwest Services outcomes and public reports, including the Wisconsin Hospital Association.
Need a tailored 2025 staffing strategy?
Let’s talk.
